Patients with chronic liver disease often face a lifelong path of decisions about their care throughout their lives. These patients stand to benefit greatly from clear, intentional conversations that help them identify their priorities and make informed decisions — even early in the treatment journey. Conversations about goals of care have several benefits, including increased quality of life, increased quality of dying, reduced intensity of care at the end of life, and reduced distress among family. Unwanted interventions can be avoided, and relationships between patients and their care teams are strengthened. Additionally, palliative care is recommended by AASLD as part of routine care, but misunderstanding from both clinicians and patients stops patients from benefitting from this valuable tool.
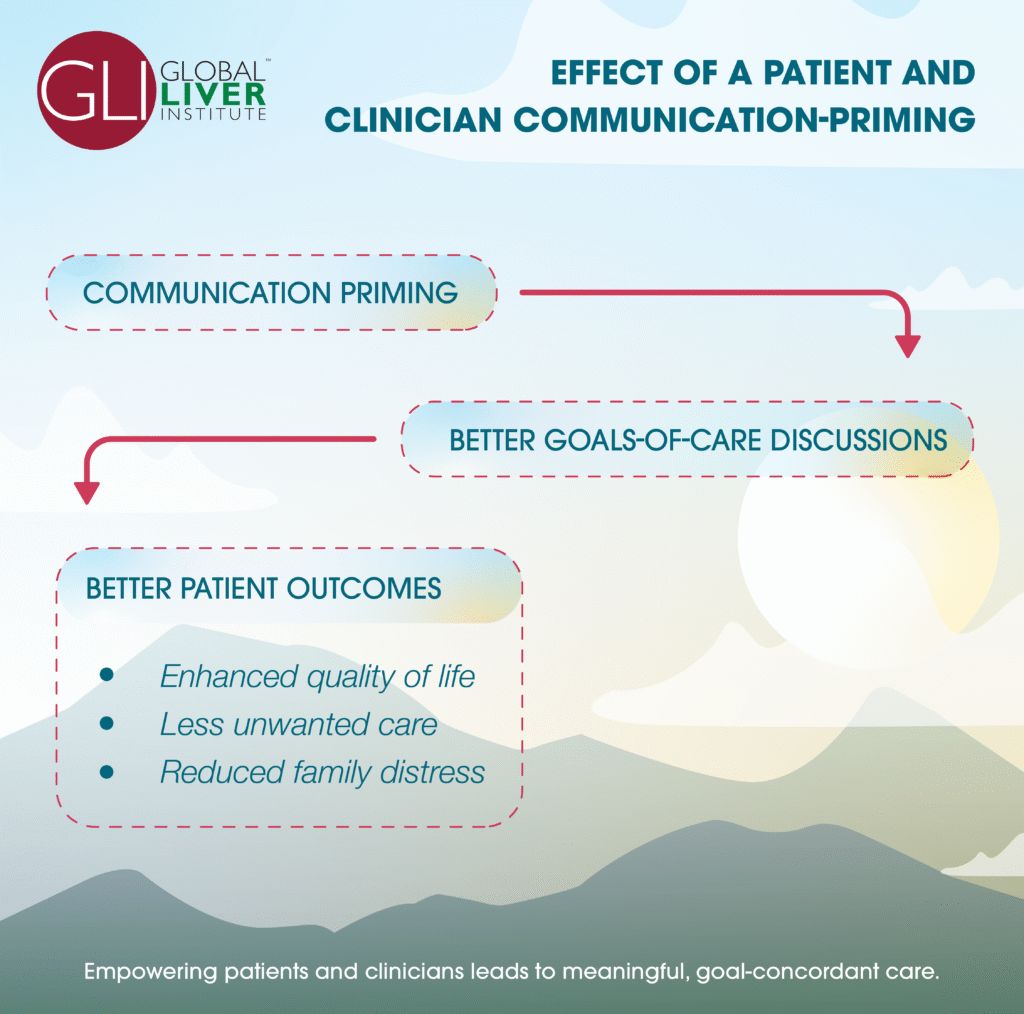
However, clinicians caring for patients with serious illness do not frequently talk about prognosis and goals of care. The timing and mechanics of these conversations are often unfamiliar. As demonstrated in a recent PCORI-funded study, a patient-specific, communication-priming intervention can successfully increase the proportion of goals-of-care conversations and resulting impact.
The intervention included patient- and provider-centric tips and videos on how to use goals-of-care among a population of patients with many types of chronic, life-limiting illnesses. Physicians and nurse practitioners providing primary or specialty care were recruited from 2 large healthcare systems in the Pacific Northwest. Study staff identified eligible patients using EHR records and contacted eligible participants by mail or telephone. Participants in the intervention arm received a survey designed to identify their preferences, barriers, and facilitators for communication about end-of-life care; based on these results, an algorithm was developed to summarize preferences and provide tailored communication tips from the VitalTalk curriculum. These tips were provided to both patients and providers 1-2 business days before the patient’s visit to prime them for a brief discussion of goals of care during the routine visit. The control arm received surveys, but no customized tips were provided to clinicians or patients.
Though clinician participation rates did not differ by general demographic categories, it did differ by specialty, with higher rates in pulmonary medicine and oncology and lower rates in family practice. Patient participation rates were not affected by demographics.
Upon the conclusion of the study, the intervention was associated with increased occurrence and quality of goals-of-care discussions. Additionally, after the visit, a significant effect on goal-concordant care was observed three months after the initial visit in patients whose goals were stable (p=.03). Depression and anxiety did not vary significantly between intervention and control groups.
Qualitative data collected suggested that the intervention was viewed as helpful, increased awareness, and assisted in opening the discussion. Particularly for patients with stable and consistent goals, facilitating conversations about goals of care helps clinicians design care that helps patients achieve these goals. Despite concern, the discussions did not lead to a significant increase in depressive or anxious symptoms.
The success of the study may be related to the self-selection of both clinician and patient participants; individuals more interested in participating may be more willing to both have a conversation and respond in kind. Still, clear value was demonstrated in achieving patient-centered care. Further studies are needed to investigate this approach in different settings.
For more information or tools for preparing for goals-of-care conversations with your patients, please review the following resources:
- Effect of a Patient and Clinician Communication-Priming Intervention on Patient-Reported Goals-of-Care Discussions Between Patients With Serious Illness and Clinicians: A Randomized Clinical Trial
- VitalTalk evidence-based skills training courses
- Goals of Care Sample Patient Guide (Humber River Health)
- Tools for Clinicians – Ariadne Labs
- Tools for Patients and Caregivers – Ariadne Labs
The statements and opinions presented in this blog post are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors, or the Methodology Committee.
