This month’s blog post is presented by Dr. Dennis Cryer, GLI Board Member, Chief Medical Officer of CryerHealth, and a former faculty member of the Children’s Hospital of Philadelphia. His experience in caring for and developing innovative therapies for vulnerable populations is instrumental to expanding the understanding of and access to vaccines.
By Dr. Dennis Cryer
Advocacy campaigns for vaccinations are primarily focused on children. However, adults, particularly those with immune systems suppressed by medications or disease such as transplant or AIDS, are greatly impacted as well.
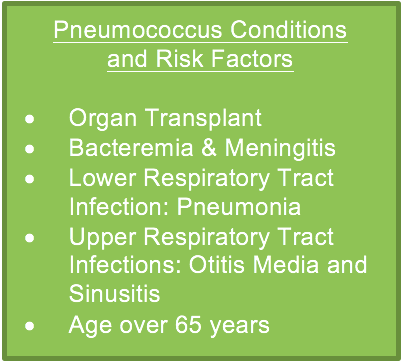
Despite recent headlines about the benefits of vaccinations at fighting disease, many adults still aren’t up to date on their shots. Without immunizations, immunocompromised adults are at high risk for certain diseases such as pneumococcal disease, meningitis, tetanus, shingles, and pertussis/whooping cough–diseases that cause pain and potentially death.
For adults living with a chronic disease like liver disease, the risks of being under-vaccinated are even greater. Statistics show that as many as one-third of adults living with a chronic illness are at greater risk of contracting the potentially deadly pneumococcal disease. Worse, if a person living with liver disease contracts pneumococcal disease, the long-term potential for worsening of their disease is elevated.
Persons with chronic liver disease have impaired phagocyte function and defects in opsonizing antibody. They may also have splenic dysfunction if the liver disease is severe. Hepatic encephalopathy or chronic alcohol consumption may lead to aspiration pneumonia. Newly acquired hepatitis A or hepatitis B in persons who already have chronic liver disease from another cause could lead to more severe disease and rapid hepatic decompensation. Those with ascites have an altered immunoglobulin production and distribution.
Vaccinations, such as the pneumonia vaccine, have been shown to save lives and protect immunocompromised individuals from developing more complex comorbid conditions. Liver disease patients experience an increased risk of nosocomial exposure to vaccine-preventable diseases due to the increased likelihood of prolonged hospitalization and frequent outpatient visits associated with their chronic disease. The earlier the vaccination is administered to an immunocompromised patient the better their response. Since individuals with chronic liver disease may experience a less than optimal response to immunization, higher vaccine doses and re-immunization may be required. As liver disease becomes more advanced, the patient will require additional vaccines, different doses, or higher dosages of vaccines to provide adequate protection.
Early vaccination is also more affordable in the long-term. Many people do not realize that vaccines are among the most successful and cost-effective public health tools available for reducing healthcare costs, morbidity, and mortality from vaccine-preventable diseases.
The CDC’s Advisory Committee on Immunization Practices (ACIP) recommends the pneumonia vaccine for all children younger than 5 years old, all adults 65 years or older, and people 6 years or older with immunocompromising conditions. The course of the 2016 election could have been affected when Secretary Clinton, in a high-risk group based on age, succumbed to pneumonia and needed to suspend her campaign. Pneumonia is ranked as one of the top 10 leading causes of death in the U.S.
However, adults aged 19-64 with risk factors such as liver disease, heart disease, asthma, diabetes and other chronic conditions are also at a higher risk of contracting the disease. Those living with a second chronic condition increase their risk contracting pneumococcal disease even further. In 2014, CDC reported the age-adjusted death rate for influenza and pneumonia as 20.9 per 100,000 U.S. standard population. Patients with chronic liver disease are at an increased risk for pneumococcal disease and its complications.
Donna Cryer, CEO of the Global Liver Institute (GLI), emphasized the importance of vaccination as a member of an ASCO Clinical Opinion on hepatitis B virus screening for patients with cancer before therapy. The publication focuses on the importance of testing for HBV and if results are negative initiating antiviral prophylaxis. In patients with chronic HBV infection, HBV treatment, review and update of all vaccinations before cancer therapy is advised. Since reactivation of latent infections has major clinical impact, antiviral prophylaxis is an attractive approach for patients expecting immunosuppression.
To target this issue, the American Association for the Study of Liver Diseases (AASLD) and the American Society of Transplantation released the 2013 Practice Guideline for liver transplant recipients recommending an annual influenza vaccination before and post-transplantation. Public health officials, health care personnel, and primary care providers in addition to specialists are in a pivotal position to ensure increased access to vaccination by administering vaccines in-clinic or amplifying education and availability of vaccination locations to patients. Liver disease specialists should educate patients and members of their household on the importance of vaccination and on infection control practices, including vaccination of household members for the protection of the immunocompromised patient.
As we raise awareness for vaccination we must also highlight goals for closing the gaps in access to treatment and prevention for immunocompromised population, including:
- Expanding the understanding of the basic aspects of vaccines in various categories of immunocompromised patients, including the epidemiology of vaccine-preventable infections, mediators of vaccine protection and adverse effects of vaccines, and effects of vaccines that contain new adjuvants on vaccine protection and adverse effects of vaccines.
- Encourage the uptake of vaccines offered by subspecialists compared with primary care providers and other strategies to increase vaccine uptake in immunocompromised patients.
- Use social media and point of care information reminding patients to maintain an up-to-date vaccination record, and if they are immunosuppressed, encourage them to ask their doctor how the normal schedule or selection of vaccinations should be modified for them.
- Technology linking Electronic Health Records, Personal Health Records, and Retail Vaccination reminders and delivery of vaccination of immunocompromised vaccine recipients, particularly those receiving live vaccines, which would also provide additional safety data.
For more information on care coordination for liver disease patients that want to ensure their vaccinations are made a priority and appropriately administered, please refer to GLI’s guidance supported by the Medicare Advantage Care Coordination (MACC) Task Force.

