This month we are fortunate to feature one of the world’s leading patient innovators, Robin Farmanfarmaian–this is no exaggeration, her book, The Patient as CEO, was a number one best seller on Amazon within days of release and has already been translated into Farsi in just its first two months in print. Robin Farmanfarmaian is a futurist, entrepreneur and speaker who has worked on over 10 tech startups, 3 as one of the founders. As a teenager, she was misdiagnosed with an autoimmune disease that led to 43 hospitalizations, 6 major surgeries, and 3 organs removed – many of them ultimately unnecessary. Robin’s unique personal history inspired her to write The Patient as CEO as an education tool and resource for healthcare professionals, the tech industry, and most importantly – patients.Please join us as Robin leads us into the possible, and indeed a necessary approach, to the shortage of solid organs for transplantation. Over 121,000 people are waiting for a vital organ transplant as of today. However, there were only 28,000 transplants performed in 2015.
Biological 3D Printing
By Robin Farmanfarmaian

The next frontier in the world of 3D printing is biological 3D printing, also known as tissue engineering. Imagine a world of on-demand 3D printed organs, made from the patient’s unique stem cells, eradicating the risk of organ rejection and the need for rejection medications.
Scientists around the world are working to solve this problem and are making headway. Right now, 3D printed liver assays – tiny working livers – are being used to test drug toxicity. A tiny patch of human liver cells are grown on a 3D scaffold inside a bioreactor. These cells react to drugs much as a liver inside you would. This is a huge step forward for drug development. No longer do drugs have to be extensively tested on living animals and humans to see if they might be toxic to the liver. They can be quickly tested using a liver assay instead. This is also a huge step forward into fully scaled, human replacement tissue engineered organs.
Tissue engineering to build organs could help reduce or even eliminate the need for traditionally transplanted organs. We already have a shortage of transplant organs that will only get worse in the future. Right now, many organs come from people who die in car and motorcycle accidents. In the future, autonomous cars will mean far fewer fatal accidents, which in turn means even fewer organs for transplant. At the Organ Preservation Alliance, a non-profit I co-founded, we’ve been working in this area of transplants with the Department of Defense, OSTP and DARPA to help make massive amounts of funding available for labs that are working on organ preservation and tissue engineering. With fewer organs available, it becomes even more urgent to learn how to preserve the current donated ones and grow new organs instead.
Scientists are making some amazing progress in replacement body parts.
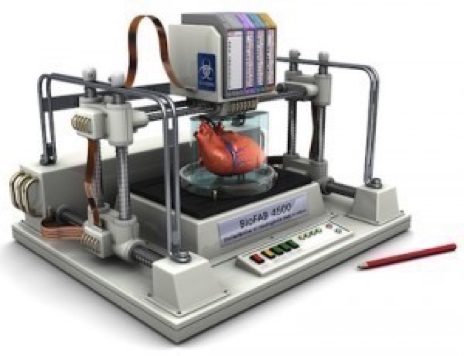
It’s now possible to grow hollow organs such as bladders and some types of cartilage, such as ears and noses. Nina Tandon’s company EpiBone grow bone grafts from the patient’s own stem cells. We can currently grow things like the liver assay cells, as well as kidney assays, because they don’t need a dense network of blood vessels to survive. Full-size vascular organs such as hearts, kidneys, and livers are much more complex. They need to have oxygen and nutrients delivered to every cell. One possible way scientists are exploring solving this problem is to take an existing organ such as a liver and decellularize it—remove all the cells but leave behind the supporting structures and blood vessels as a scaffold. Stem cells could then be used to populate the scaffold and grow a new liver. We can successfully do that now with the bladder because it’s basically hollow, but bigger, more complex organs will take more work.
Complex blood vessels are another area where 3D bioprinting has huge potential for breakthrough technology. At the Wyss Institute for Biologically Inspired Engineering at Harvard University, Jennifer Lewis leads a team that has figured out how to print blood vessels in tissue using disappearing ink.
The tissue is built up in layers with a 3D bioprinter. The “inks” are viscous gelatins that contain structural supports and living cells. To make the blood vessels, a different type of gelatin is used, one that is viscous at room temperature but liquid when it’s cooled. This ink is used to print blood vessels within the cell layers. When the patch of tissue is cooled, the “invisible ink” of the blood vessels is gently sucked out, leaving the channels behind. Epithelial stem cells, the kind that make the linings of blood vessels, are seeded into the channels, where they will grow into working capillaries.
What’s the timeline?
When I ask scientists what they think the timeline is for fully tissue engineered organs, I hear a range of 15-25 years. There are lots of hurdles, including the regulatory environment, even after this life-giving technology is perfected.
The potential for this technology to be a game-changer for humanity is very clear. Organ failure is the number one killer in the US. About 35 percent of deaths in the U.S. could be significantly delayed or prevented through an organ transplant–that’s roughly 900,000 people a year who are affected. Imagine a world where instead of repairing an organ or treating a disease with medication, you just switch out your organ, grown from your own stem cells. Things that may seem like pure science fiction are becoming a reality.

Visit Robin’s website at http://robinff.com and follow her on Twitter @RobinFF3.
