Smart Tools, Healthier Livers: How Digital Health Can Help You Take Control

Smart Tools, Healthier Livers: How Digital Health Can Help You Take Control
Whether you know it or not, your liver plays a central role in your health. It has over 500 functions in the body, including filtering toxins from the blood and helping manage levels of sugar and cholesterol in your blood.
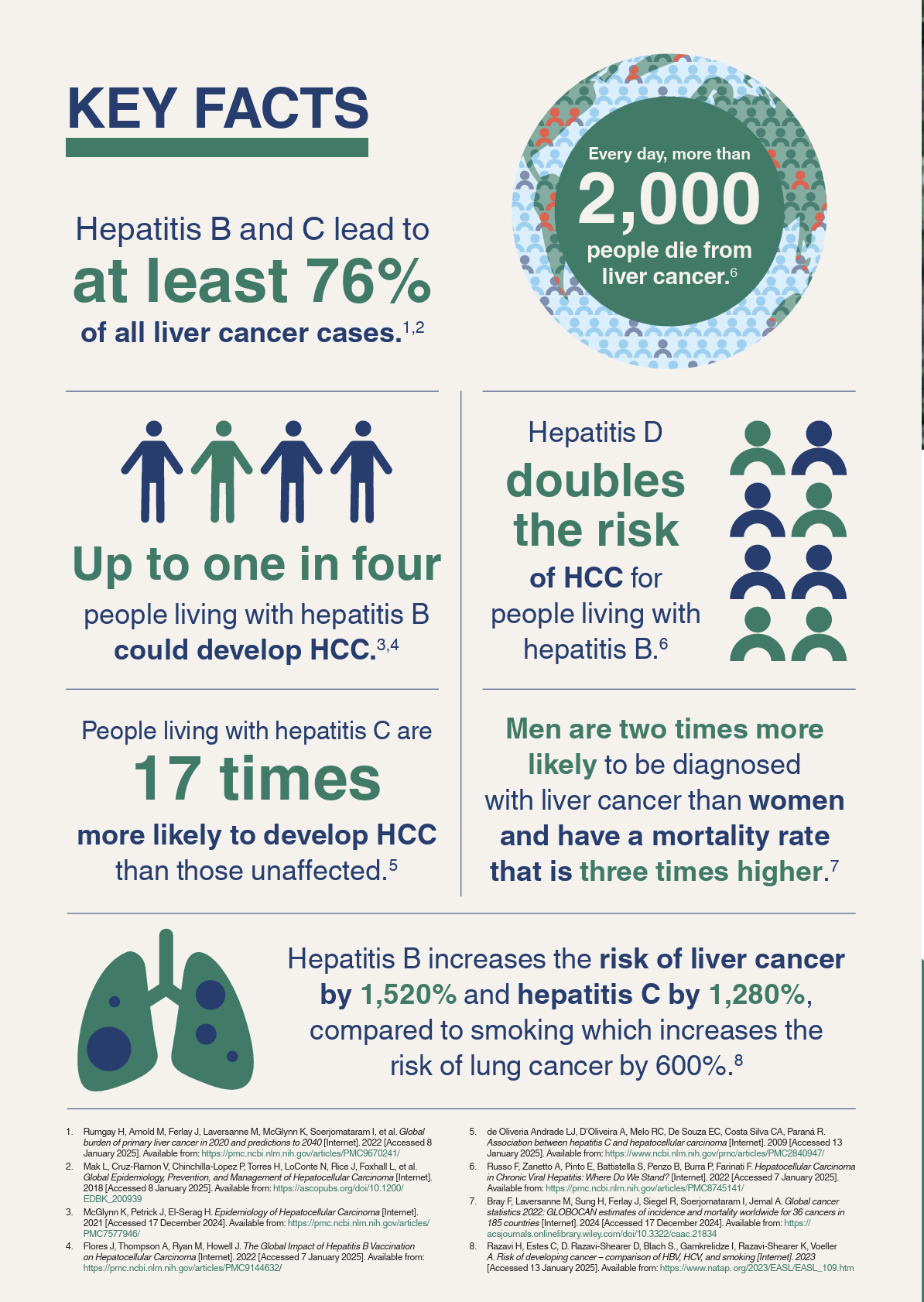
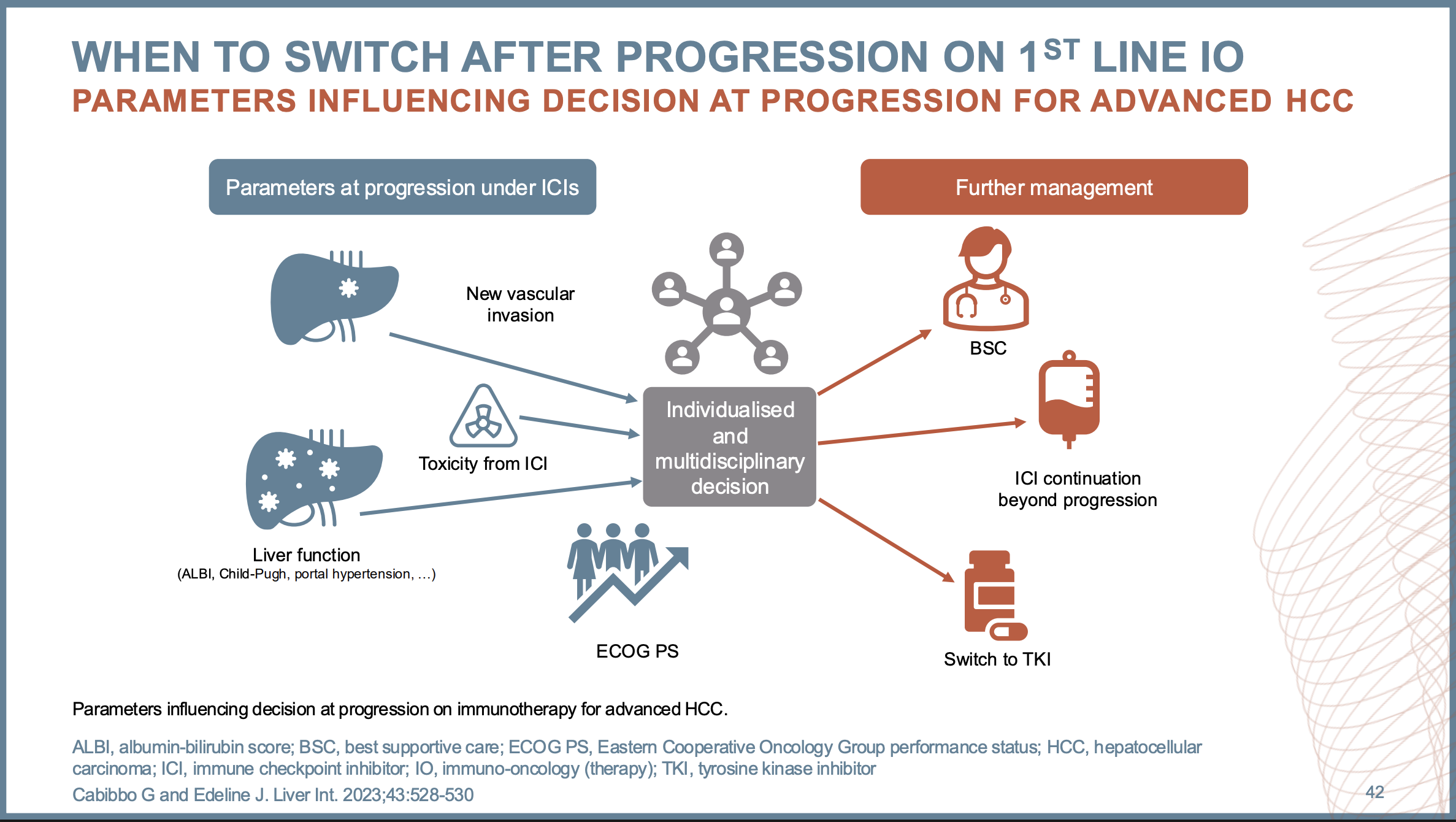
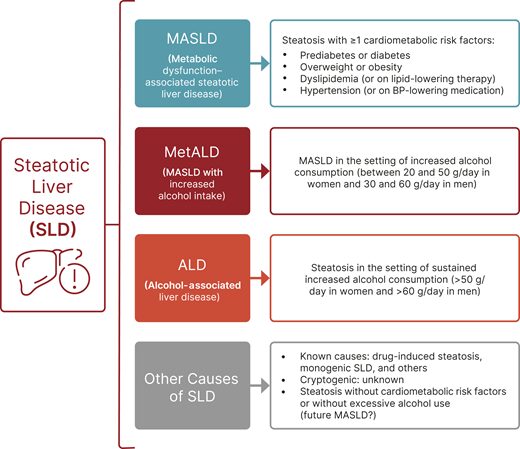
Technology is changing how we manage our health, liver health included. Whether you are screening for or managing a chronic condition like metabolic dysfunction-associated steatotic liver disease (sometimes called “fatty liver disease”) or viral hepatitis or proactively protecting your liver health, many digital tools can help you stay informed, track your health, and manage your care – right from your phone or computer. Here are a few trusted, digital tools that can keep you in control of your health:
Patient Portals: Health Dashboard and Message System in Your Pocket
Patient portals (like MyChart) are secure, internet-based platforms provided by your hospital or clinic that allow you to access your electronic medical records, communicate with your healthcare providers, and manage your full care journey, from appointments to health information. Many patient portals allow you to:
- Track lab results (like your liver enzyme levels)
- Message your doctor or nurse
- Request prescription refills
- Schedule referred appointments with specialists
- Book or adjust appointments
- View appointment history
By staying on top of your lab results and follow-up appointments and consolidating your health information, you can help ensure that any liver issues are detected early and managed promptly. All the while, you and your care team have a complete picture of your health.
Educational Apps: Trusted Information at Your Fingertips
Not all information available on the internet is created equal. When navigating care for yourself or a loved one, it is easy to become overwhelmed by the deluge of information available.
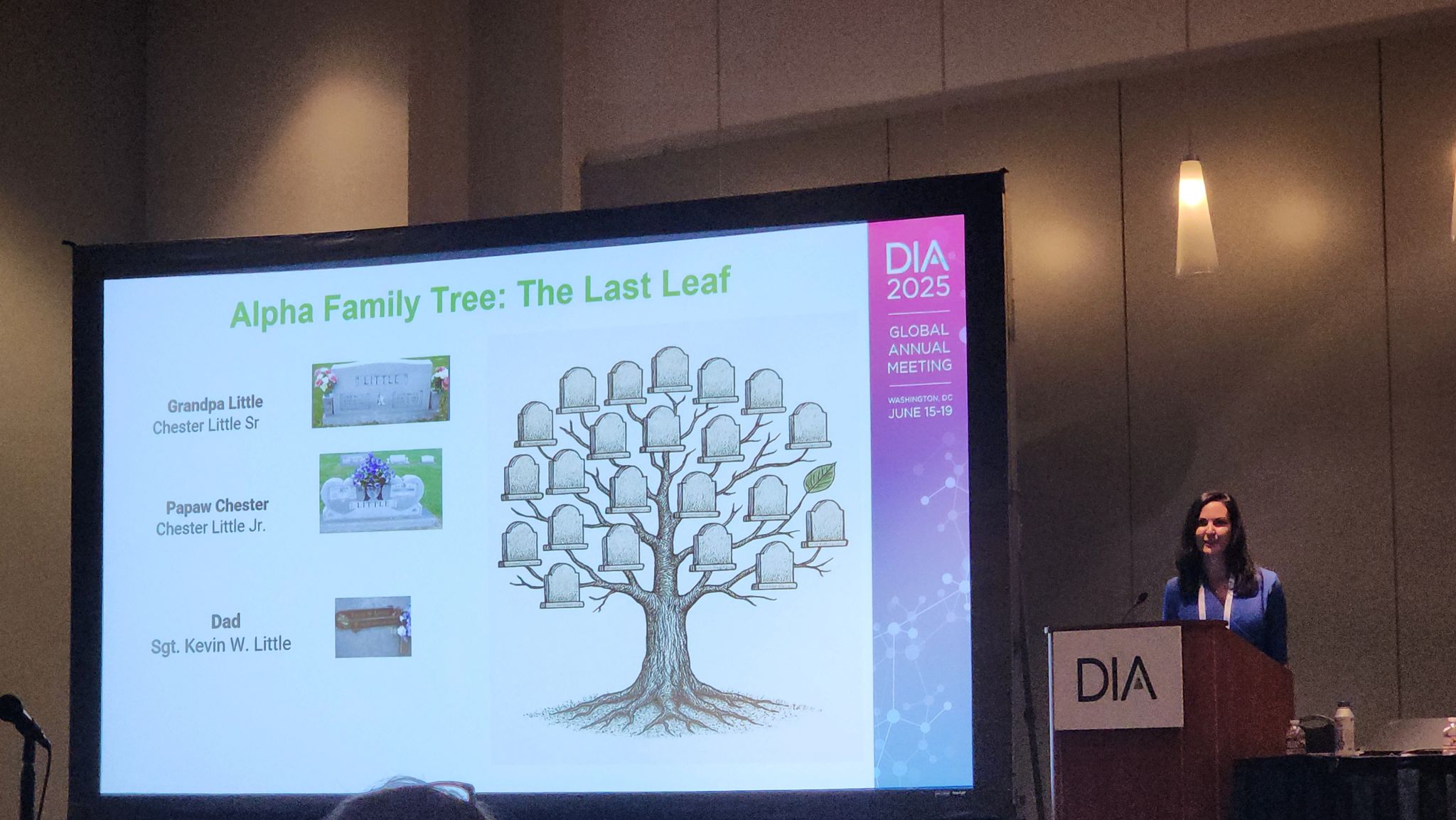
Many clinics offer clinically vetted, evidence-based educational apps, whether within the patient portal or as standalone resources, corresponding to the risks or diagnoses you might have. One great example is the Hepatitis App, investigated in the “Health Within Reach” study. This app, designed specifically for and alongside Asian-American communities, offers culturally and linguistically appropriate videos about hepatitis B and the importance of immunization and screening. By providing targeted information to groups with heightened risk in patients’ native language, clinics were able to increase screening rates and provide needed treatment.
Ask your care team for resources, and look for apps created by government agencies, hospitals, universities, reputable nonprofit organizations, or public health organizations. Avoid anything that makes promises that sound too good to be true… like “detox your liver in 3 days.”
Medication & Wellness Trackers: Staying on Schedule
If you’ve been prescribed medication for liver disease and related conditions, or just need help remembering vitamins and supplements, several apps can send reminders, track doses, and organize your med list. Sometimes these features are integrated into your patient portal!
Lifestyle also plays a big role in liver health. Websites and apps that help you monitor your nutrition and movement, like Nutristyle or built-in apps like Apple Health and Google Fit, and others support goals like reducing sugar, maintaining a healthy weight, or limiting alcohol, all of which protect your liver.
Virtual Visits: Liver Care From Home
Telehealth lets you connect with liver specialists from the comfort of your home. For people in rural or underserved areas, without many clinics or specialists, this option can be especially helpful for follow-up visits and check-ins.
If you have a smartphone, tablet, or computer, ask your doctor’s office if telehealth is an option.
The Power of Connection: Online Support Communities
Liver disease is often stigmatized, which can be extremely isolating, but digital platforms make it easier to connect. Online communities can offer support, encouragement, and shared experiences. Peer support is shown to reduce isolation and increase motivation to take the steps necessary to promote your health!
If you’d like to be connected to an online community related to a diagnosis you have, please email our team at info@globalliver.org, and we can connect you to one of the groups that we trust.
Remember: As valuable as peer support can be in your health journey, it does not replace professional guidance. Always double check medical advice with your healthcare provider before making major changes.
A Word about the Digital Divide
Not everyone has equal access to the internet, devices, or tech know-how. Some people may not have internet at home, or may feel unsure about using apps and online portals. That’s completely understandable – and you’re not alone.
Your local library can help. Many offer free internet access, computer use, and even digital literacy classes. Some libraries have staff who can walk you through how to set up your patient portal or download a health app. Don’t be afraid to ask.
~ ~ ~
Whether it’s signing up for your patient portal or downloading a trusted app, digital tools can help you stay on top of your liver health – and feel more in control of your care.
The statements and opinions presented in this blog post are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors, or the Methodology Committee.