Join GLI in Supporting the LIVER Act!
GLI is thrilled to share that Representative Nydia Velázquez has reintroduced the Liver Illness, Visibility, Education and Research Act (LIVER Act). The bill was first introduced in 2018, in collaboration with GLI in its development. With rising rates of liver cancer, fatty liver disease and new opportunities to prevent and treat viral hepatitis, GLI believes the time is now for Congress to move the field forward and shift the conversation to shine a spotlight on liver cancer and liver health disparities. View GLI’s statement here. Join us by reaching out to your Member of the House of Representatives here!
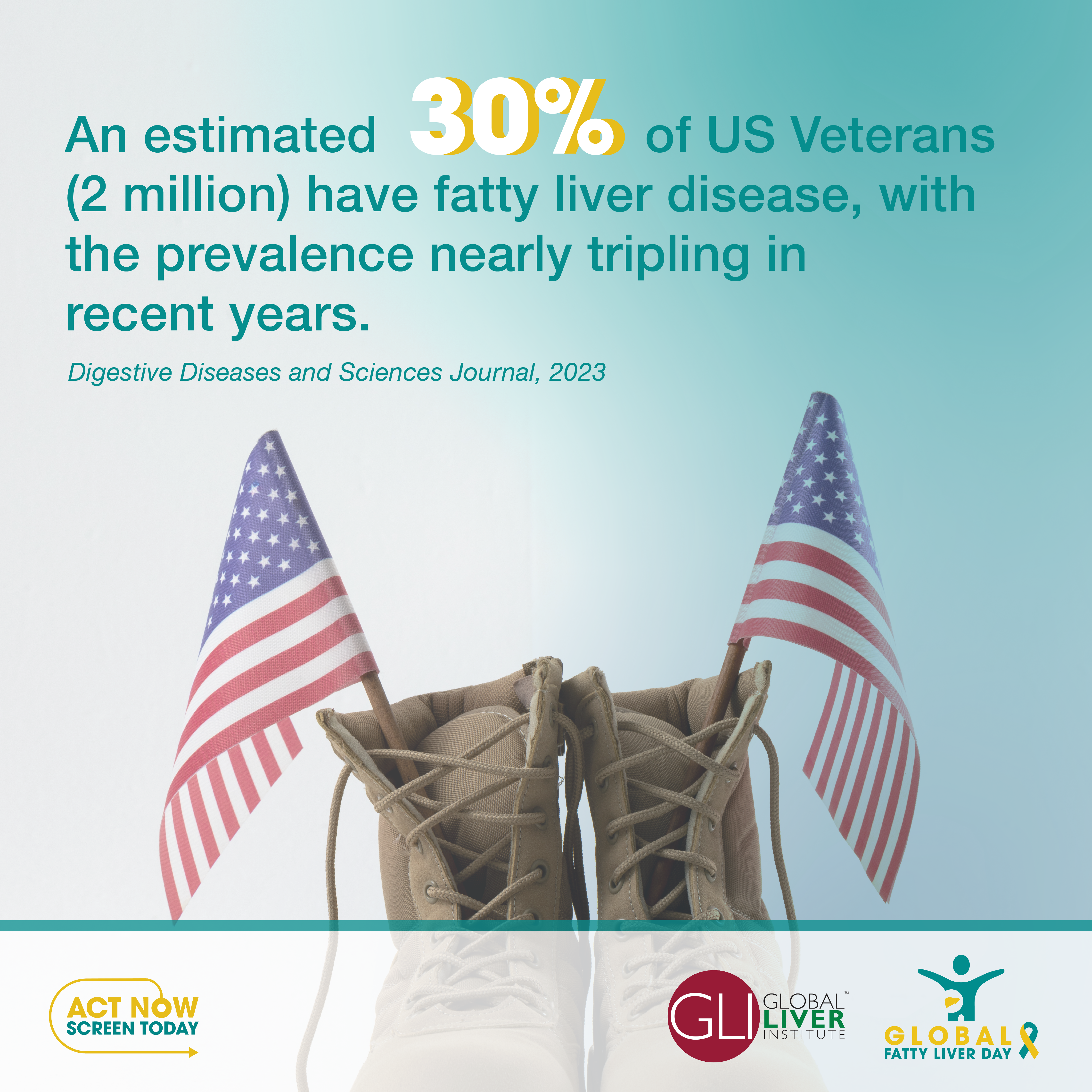
GLI Pushes for Access to NASH/MASH Treatment for Veterans
GLI and 24 organizations sent a letter to the U.S. Department of Veterans Affairs expressing deep concern that the agency is advancing adverse Criteria for Use of a new medication to treat nonalcoholic ateatohepatitis (NASH), also known as metabolic dysfunction-associated ateatohepatitis (MASH), to include biopsy, contrary to the label from the Food and Drug Administration and clinical guidelines. Groups also expressed concern that the VA’s recommendation on lifestyle interventions will further delay access to care. The VA did not provide any information on the evidentiary basis for this decision, nor is it supported by existing clinical guidelines. The letter urged the VA to remove the VA Pharmacy Benefits Management Services and National Formulary Committee’s recommendation of biopsy as a Criteria for Use for any approved medication for NASH/MASH. Click here to view the letter. Click here to learn more about Beyond the Biopsy.
GLI Supports the Old Drugs New Cures Act!
Congressmen Don Davis (D-NC) and August Pfluger (R-TX) have introduced the Old Drugs New Cures Act, bipartisan legislation to improve access to lifesaving medications that disproportionately benefit low-income Americans who rely on Medicaid, the Children’s Health Insurance Program (CHIP), or Medicare Part D low-income subsidies (LIS). As GLI’s Donna R. Cryer, JD, points out, “reformulating existing drugs is an opportunity for innovation to address unmet needs in an efficient and timely manner.” New uses for existing drugs have long been supported by the rare disease community, for whom treatment options are highly limited. The bill remedies an interpretation of federal law that stifles research and development on reformulations of existing drugs for new uses, called the Medicaid line extension. The bill carves out an exemption for priority research drugs from the Medicaid line extension, allowing for a smoother path from drug development to patient access. View the press release here.
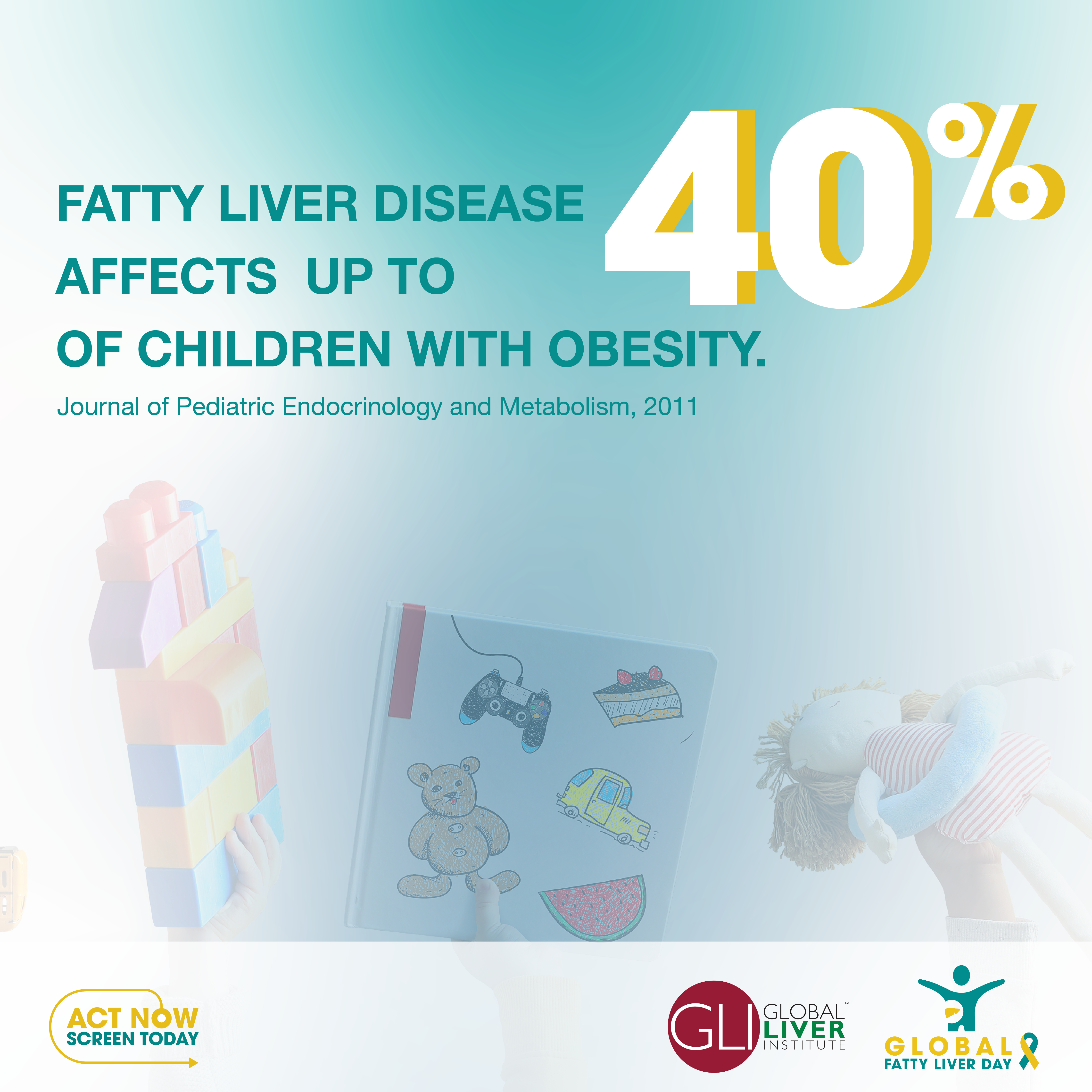
GLI Urges New York to Cover Obesity Drugs
GLI strongly supports Medicaid policies addressing the chronic disease of obesity that are based on sound science and support health equity. It is critical for state policies to recognize obesity as a serious and complex condition that is a risk factor for developing NASH/MASH. While we applaud the State of New York for providing access to medication treatment for obesity to NY state employees, we are concerned that the population currently lacking access to the full array of obesity treatments is the state’s Medicaid population. The disparity in coverage is stark and contrary to the state’s goals for health equity. Prevention not only saves live but would save money and hardship by addressing the personal and financial burden of obesity and related diseases and conditions for so many people and families. GLI sent a letter to the Governor asking that new obesity treatments no longer be excluded, and sent letters to the New York Senate and Assembly supporting legislation to provide comprehensive coverage for obesity care.
GLI Appeals to Biden Administration to Provide Comprehensive Care for Obesity
As part of a continuing strategy to provide access to comprehensive obesity care, 58 organizations urged the Biden Administration to add obesity into the category of complex, chronic disease states under the National Strategy on Hunger, Nutrition, and Health guidelines. GLI also urged the Biden Administration to provide Medicare Part D prescription drug coverage of obesity medications and expand the type of qualified healthcare and community providers and evidence-based community programs that can deliver intensive behavioral therapy (IBT) under Medicare Part B. Click here to view the letter signed by 58 organizations. Click here to send a letter!
Bipartisan Congressional Preventive Health and Wellness Caucus Launched!
Congressman Vern Buchanan, Vice Chairman of the House Ways and Means Committee and Chairman of the Health Subcommittee, and Congresswoman Gwen Moore (D-WI) announced the launch of the bipartisan Congressional Preventive Health and Wellness Caucus. The caucus will work to bring awareness to the burgeoning obesity epidemic in the country and help promote and advance policy-centric solutions. Specifically, the bipartisan group will focus on the effects of prevention, Medical Research and Innovation (MRI), Food as Medicine (FAM), exercise, health disparities, coverage, stigma, and obesity on military readiness and physical fitness. In your advocacy, please join GLI in encouraging Members of the House of Representatives to join the caucus and support policies such as the Treat and Reduce Obesity Act providing comprehensive coverage for obesity treatment! Reach out to your Member of Congress here.
DOD Responds to GLI Outreach Supporting Obesity Care for the Armed Forces
GLI is proud to support decisive action by the U.S. Department of Defense to rectify systemic issues preventing individuals with obesity from accessing evidence-based treatments including behavioral therapy, AOMs, and bariatric surgery. GLI and other advocacy organizations sent a letter to DOD, available here. We are pleased to report that the return letter to the American Security Project from DOD stated that the Secretary agrees that obesity poses a threat to our national defense, supports our aims and purpose, and is reviewing our recommendations and suggestions in more detail. We are encouraged by this response, which represents a huge step forward in improving medical care for our service members and veterans. It is important to note that neither overweight nor obesity are currently classified as chronic diseases in the Active Duty, which makes the Secretary’s decision to explore this recommendation critical to improved identification and treatment of these conditions. View the press coverage from Federal News Network, Military Times, and Daily Express.
GLI Applauds House Energy and Commerce Health Subcommittee Action on Telehealth
GLI has consistently supported access to telehealth as a key strategy for improving relationships between doctors and patients that allows patients to actively show doctors their medicine bottles, the environment in which they live, and even the contents of their refrigerators. Doing so allows doctors to better understand how to tailor a treatment plan around a patient’s real-world circumstances and thus improve treatment adherence. On May 16, the House Energy and Commerce (E&C) Subcommittee on Health held a markup on a series of substantial health-related proposals geared towards extending access to telehealth services, strengthening and preserving the Medicaid program, and encouraging innovation for pediatric rare diseases. 21 pieces of legislation were ultimately reported favorably, 18 of which had unanimous support. Notably, committee Democrats leveraged the markup’s discussions on telehealth legislation to urge their Republican colleagues to also reauthorize the soon-to-expire Affordable Connectivity Program (ACP).
Senate Holds Hearing on Food is Medicine
On May 21, 2024, the Senate Health Education Labor and Pensions (HELP) Committee held a hearing on Feeding a Healthier America: Current Efforts and Potential Opportunities for Food is Medicine. Nutrition experts emphasized that providing nutritious meals to vulnerable populations can save lives and curb healthcare costs, a sentiment shared by GLI and the Liver Action Network. GLI continues to actively engage in efforts on Capitol Hill to support the Medical Nutrition Equity Act requiring insurers to cover critical medical food for patients. Share your support here!
GLI Supports NIH Funding to Address Deadliest Cancers
GLI and the Deadliest Cancers Coalition continue to support funding to address deadly liver cancers. GLI urges Congress to increase its appropriations to the NIH to $51.3 billion for the NIH’s base program budget level, including $7.93 billion for the NCI, as well as at least $1.5 billion for the Advanced Research Projects Agency for Health (ARPA-H). GLI also supports report language that continues to hold NCI accountable for making progress on the goals and ideals of the Recalcitrant Cancer Research Act and asks that NCI develop a plan with specific actions to understand the causes and risk factors that are leading to recent increases in incidence of deadly cancers, especially liver cancer. GLI also supports Congressional efforts urging NCI to consider a multi-disciplinary workgroup to report on research focus areas for primary liver cancer, including cholangiocarcinoma, and looks forward to learning more about the RFI released for liver and pancreatic cancer in January 2023. Reports of unexplained increased incidence of deadly cancers such as liver cancer among the adolescent and young adult population require the NCI’s attention to develop a plan with specific actions to understand the causes and risk factors that are leading to these increases and potential interventions. Learn more about efforts urging NIH to address deadliest cancers here.
GLI Supports Full Funding to Support FDA’s Responsibilities to Patients and Consumers
The FDA is responsible for 80% of the food supply and 100% of drugs, medical devices, biologics, vaccines, veterinary food/medicine, dietary supplements, and cosmetics in the United States. Altogether, the agency oversees products and services that represent 20% of all consumer spending (more than $3.6 trillion). GLI is proud to join the Alliance for a Stronger FDA in calling for increased appropriations to support the FDA’s activities, particularly to improve the accuracy and efficiency of FDA’s medical product decisions, address rare disease and support medical nutrition. It is not an option for the FDA to be underfunded and under-resourced. The FDA’s ability to operate a modern, scientifically-based regulatory program must be continually strengthened. View more information about the resources needed to support FDA’s work here.